How p16 Helps Detect Early Cervical Changes
2025-11-27
By admin

The Critical Need for Early Cervical Cancer Detection
Cervical cancer is one of the few cancers doctors can almost always stop if they catch the warning signs soon enough. The problem is that the usual screening tools, like the Pap smear, sometimes leave pathologists guessing. A slide might look a little abnormal, but is it the kind that goes away on its own, or the kind that turns into real cancer if nobody does anything? Too many women end up getting extra tests and biopsies they never needed, while a few others slip through with serious changes that get missed. Everybody in the lab wants something clearer—something that says “this one is safe to watch” or “this one needs treatment now” without all the gray area.
The Challenge of Conventional Cervical Screening
For years, the Pap test has been the first line of defense. A nurse scrapes a few cells off the cervix, the lab stains them, and someone looks under the microscope. Most of the time, it works fine. But when the changes are mild, deciding whether it’s just a low-grade squiggle (CIN1) or the start of something dangerous (CIN2/3) can be tough. That kind of disagreement leads to overtreatment for some patients and, worse, undertreatment for others.
The Rise of Molecular Biomarkers in Precision Diagnostics
That’s why labs all over the world have started adding special stains that look at what’s happening inside the cells, not just how they look on the surface. Out of all the new markers, one protein—p16—has become the go-to sign that high-risk HPV is actually messing with the cell’s brakes. When p16 lights up strongly across a whole patch of cells, pathologists finally have an objective yes-or-no answer.
Understanding p16: The Definitive Cervical Precancer Biomarker
High-risk HPV is behind nearly every case of cervical cancer. The virus makes two trouble-making proteins, E6 and E7. Those proteins knock out the cell’s normal control system, and p16 is the alarm that goes off when that happens.
What is p16 and Its Role in the Cell Cycle?
In a healthy cell, p16 acts like a stop sign. It keeps the cell from copying its DNA and dividing until everything is ready. Think of it as the guard that stops the cell from moving from first gear (G1) into second gear (S phase).
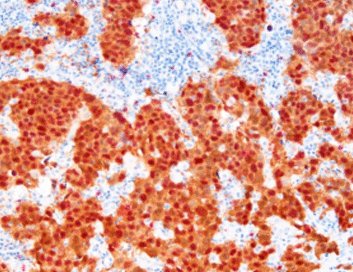
p16 Overexpression: A Reliable Sign of Oncogenic HPV Activity
When the HPV E7 protein shows up, it ties up the main brake (the Rb protein) so the cell can’t slow down anymore. The cell notices something is wrong and starts pumping out huge amounts of p16 to try to fix the problem. It’s like hitting the brake pedal after the brake line has been cut—the pedal goes to the floor, but nothing slows down. That flood of p16 is easy to see with a simple stain. Strong, widespread p16 staining almost always means high-risk HPV is actively pushing the cell toward cancer. Regular cell turnover or low-risk HPV almost never causes that kind of dramatic p16 reaction, so the signal is remarkably trustworthy.
Maximizing Diagnostic Precision: The Power of p16/Ki-67 Dual Staining
One marker is good; two are even better. Pairing p16 with Ki-67—the protein that shows a cell is actually dividing—gives pathologists a double check that’s hard to argue with. Celnovte has built its cytology lineup around this exact combination.
Differentiating Low-Grade from High-Grade Lesions
Here’s what the stains look like in real life:
-
Low-grade spots (CIN1 or less): Usually no p16 at all, or just faint patches low in the epithelium. Ki-67 is only in the bottom layer, where new cells normally grow.
-
High-grade spots (CIN2/3): Big blocks of strong brown p16 staining that go two-thirds or all the way up the epithelium, and bright Ki-67 dots in the same cells that have p16. When you see both stains lighting up the same cell at the same time, that’s the smoking gun for real precancer.
Interpreting Dual Staining: A Clear Signal for Risk Stratification
A cell that’s making tons of p16 and still dividing like crazy is a cell that has lost control. That one-two punch leaves very little room for doubt. Celnovte rolled out the [Red/Brown] P16/Ki-67 Dual Staining Detection Kit, so the two signals literally jump out under the microscope—one color for p16, a completely different color for Ki-67. Pathologists tell us it cuts reading time and cuts disagreement way down.
Celnovte’s Technological Edge: Enhancing p16 Detection
Celnovte started with a simple goal: give labs tools they can trust every single day. From antibodies to automated stainers, everything is built around making tough diagnoses easier and more reliable.
Celnovte’s p16/Ki-67 Dual Staining Solution
These kits are made specifically for liquid-based cytology slides (ThinPrep and SurePath). The antibodies are strong, the colors are crisp, and the P16/Ki67 system makes double-positive cells impossible to miss—even on a busy Monday morning when the lab is slammed.
MicroStacker Detection Systems
No matter how good the antibody is, you still need a detection system that can pick up the signal without adding background junk. The MicroStacker polymer backbone gives a clean, strong boost, so even weak p16 expression shows up clearly. The newest MicroStacker Ultra is currently the most sensitive system on the market for cytology work. Labs that switched to it report fewer repeat stains and fewer “can’t tell” cases.
The CNT480 Fully Automatic Cytology Stainer
Doing p16/Ki-67 by hand takes about two and a half hours per run, and every tech does it a little differently. The CNT480 Fully Automatic Liquid-based Cytology Immunocytochemistry Stainer runs the whole protocol with robotic precision. Load the slides, walk away, and come back to perfectly stained batches every time.

Ensuring Quality and Consistency in Pathology Workflows
When a woman’s follow-up depends on one slide, “pretty good” isn’t good enough.
Global Quality Compliance and Proven Reliability
Celnovte’s factories in the United States and China are fully NMPA & GMP compliant. They carry ISO13485, ISO9001, FDA registration, and CE IVDR marking. Forty-seven of the company’s primary antibodies have earned top or good marks from NordiQC, the independent quality group that tests antibodies blind. That kind of track record means a lab in Taipei or Toronto can trust the same bottle that a lab in Texas uses.
Elevating Results through Innovative Technology
Put the MicroStacker detection system together with the CNT480 stainer and Celnovte antibodies, and you turn a test that used to tie up a tech for half a day into a push-button routine. Labs that made the switch tell us they read slides faster, argue less at the multi-head scope, and feel a lot more confident sending out a high-grade diagnosis.
Conclusion: Precision Diagnostics for Better Patient Outcomes
At the end of the day, p16 isn’t just another stain on a long menu. It’s the clearest red flag we have that high-risk HPV has hijacked a cell and is pushing it toward cancer. When you add Ki-67 and use rock-solid tools like Celnovte’s dual-stain kits, MicroStacker detection, and the CNT480 automated platform, pathologists stop guessing and start knowing. Women get the right follow-up the first time—nothing more, nothing less. That’s how we actually lower the number of cervical cancer cases instead of just finding them earlier.
FAQ
Q: What is the main advantage of p16/Ki-67 dual staining over traditional Pap tests?
A: It’s far more specific. The Pap looks at shape; dual staining proves the cell is both driven by oncogenic HPV (p16) and actively dividing (Ki-67). That combination almost never happens in harmless changes.
Q: How does Celnovte ensure the quality of its p16 detection products?
A: Full regulatory package—ISO13485, FDA, CE IVDR—plus dozens of antibodies with top NordiQC scores and over 800 automated stainers running daily in labs around the world.
Q: What is the role of the MicroStacker™ Detection System in p16 analysis?
A: It gives the cleanest, strongest signal available, so even faint real p16 expression stands out without background noise that could confuse the reading.
Q: Can Celnovte’s automated instruments handle the p16/Ki-67 assay?
A: Yes—the CNT480 Fully Automatic Liquid-based Cytology Immunocytochemistry Stainer was built for exactly these assays on ThinPrep or SurePath slides, delivering batch-to-batch consistency that hand staining can’t match.